Introduction
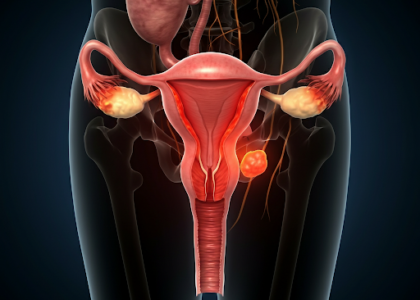
Planning Pregnancy with Diabetes: Diabetes can be a challenging condition to manage, especially when you’re planning a pregnancy. However, with proper planning, medical guidance, and lifestyle adjustments, it’s entirely possible to have a healthy pregnancy and a thriving baby. This Q&A guide addresses the most common concerns for women with diabetes who are planning to conceive.
Q&A Format
Q1. Can I plan a pregnancy if I have diabetes?
Absolutely! Women with diabetes can have a healthy pregnancy with adequate planning and care. It’s essential to have your blood sugar levels under control before conception to reduce risks for both you and your baby. American Diabetes Association: Pregnancy
Q2. How does diabetes affect pregnancy?
Uncontrolled diabetes can pose risks such as:
- For the baby: Increased risk of congenital abnormalities, premature birth, and higher birth weight.
- For the mother: Risk of preeclampsia, infections, and complications during delivery.
Q3. What should I do before trying to conceive?
Here’s a checklist:
- Consult your healthcare provider: A preconception checkup is vital.
- Manage blood sugar levels: Aim for HbA1c levels below 6.5%.
- Monitor medications: Ensure diabetes medications are safe for pregnancy.
- Adopt a healthy lifestyle: Maintain a balanced diet, exercise, and manage stress.
- Take folic acid supplements: To prevent neural tube defects.
Q4. What diet is recommended for women with diabetes planning pregnancy?
A balanced, diabetes-friendly diet includes:
- High-fiber foods: Whole grains, legumes, and vegetables.
- Lean protein: Fish, eggs, and poultry.
- Healthy fats: Nuts, seeds, and avocados.
- Controlled carbs: Small, frequent meals to prevent sugar spikes. Lifestyle Tips for Reproductive Health
Q5. How often should I monitor my blood sugar levels during pregnancy?
Frequent monitoring is key. Most doctors recommend checking:
- Before meals.
- 1-2 hours after meals.
- At bedtime.
Q6. What are the risks of uncontrolled diabetes during pregnancy?
- Gestational hypertension: High blood pressure during pregnancy.
- Macrosomia: Excessive fetal growth leading to delivery complications.
- Miscarriage or stillbirth: Increased risk if blood sugar is not managed.
Q7. What medical support do I need during pregnancy?
- Regular prenatal checkups: To monitor baby’s growth and your health.
- Specialist consultations: Work with a diabetologist or endocrinologist.
- Ultrasounds and fetal monitoring: To track development and prevent complications.
Q8. Can gestational diabetes occur if I already have diabetes?
No, gestational diabetes specifically refers to diabetes that develops during pregnancy in women without a prior history of diabetes. However, women with diabetes can experience challenges in maintaining stable blood sugar levels during pregnancy.
Q9. Are insulin injections necessary during pregnancy?
Many women with diabetes rely on insulin during pregnancy as it is safe and helps maintain tight blood sugar control. Your doctor will advise whether insulin is needed or if oral medications suffice.
Q10. What post-pregnancy precautions should I take?
- Monitor blood sugar levels after delivery.
- Breastfeed, as it helps regulate blood sugar and provides nutrition for your baby.
- Attend postpartum checkups to address any complications.
Conclusion
Planning pregnancy with diabetes requires careful preparation and collaboration with your healthcare team. By managing blood sugar levels, following a healthy lifestyle, and staying informed, you can enjoy a safe pregnancy and a healthy baby.
Call to Action:
For personalized guidance on planning pregnancy with diabetes, visit our Home – Dr. Anjana Jain | Gynae Clinic or book an appointment at 9453951849 today.





Recent Comments